New Guideline for Using Lab Tests to Improve Cancer Treatment
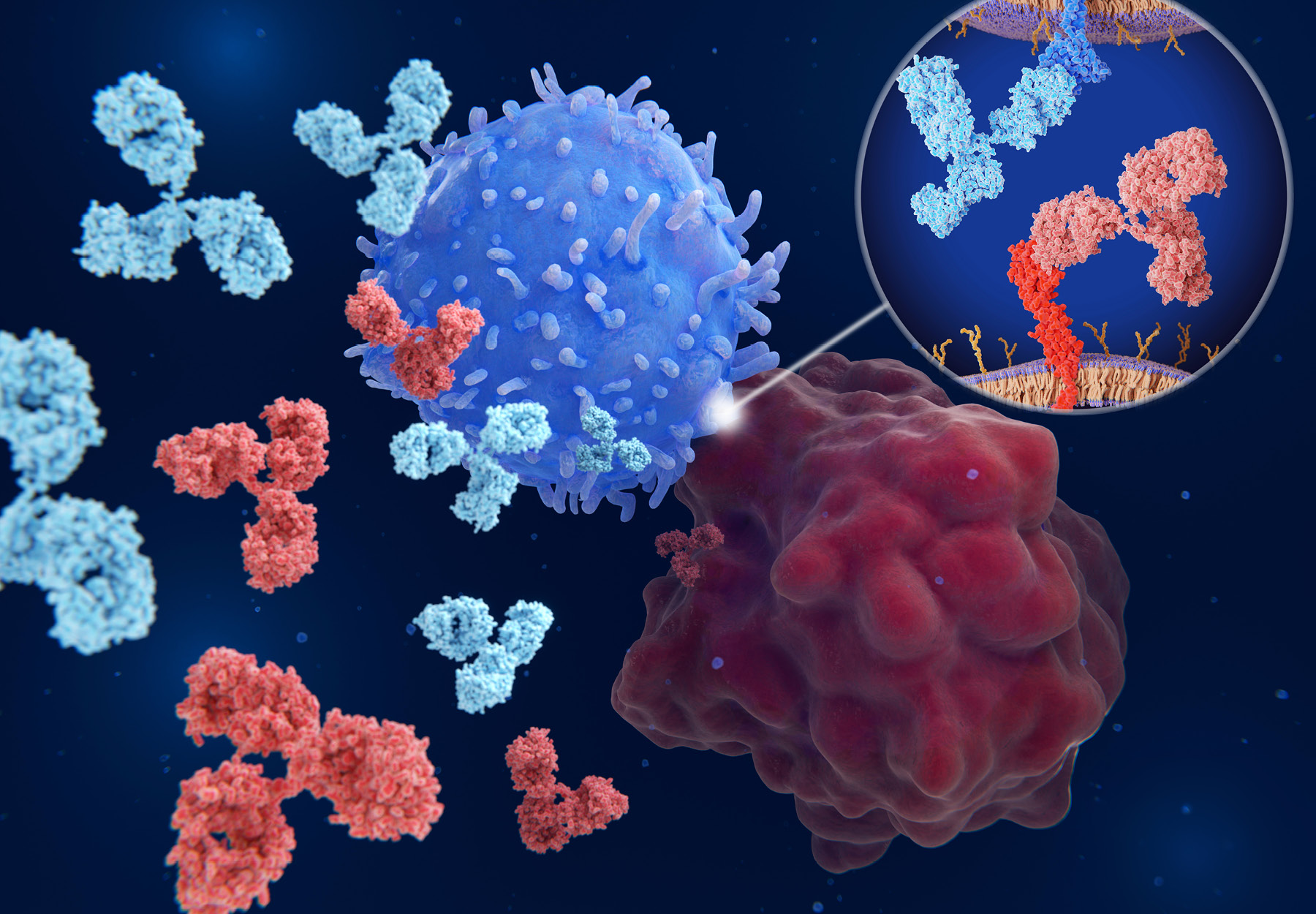
The new CAP guidance addresses use of immune checkpoint inhibitors for evaluating and treating patients with specific cancers.
Subscribe to Clinical Diagnostics Insider to view
Start a Free Trial for immediate access to this article