Early in Pandemic, HIV Testing Dropped Sharply, but Quickly Rebounded
A recent CDC report concludes that disruptions to HIV testing due to the COVID-19 pandemic compromised America’s ability to prevent the disease.

The massive disruptions to HIV testing during the COVID-19 pandemic compromised the nation’s ability to prevent the disease and highlighted the need for long-term planning and innovative diagnostic solutions before the next public health emergency strikes. That is the conclusion of a new report published by the US Centers for Disease Control and Prevention (CDC) on December 1, 2022.1 Here is a quick briefing on the CDC analysis and its potential implications for future laboratory testing.
The Diagnostic Challenge
In February 2019, the Trump administration announced the launch of the federal Ending the HIV Epidemic in the U.S. (EHE) initiative, with the goal of reducing new HIV infections by 90 percent by 2030. The EHE calls for the increased use of three key methods for diagnosing, preventing, and treating HIV:2
-
- HIV laboratory testing;
-
- Pre-exposure prophylaxis (PrEP); and
-
- Antiretroviral therapy (ART).
The EHE was widely embraced as a positive step forward. What nobody foresaw at the time was how the COVID-19 public health emergency that was declared one year later in March 2020 would throw the EHE strategy into disarray. Lockdown orders kept people from leaving their homes. Nonessential businesses, including most nonemergency healthcare venues, closed down. Employees got laid off, often resulting in the loss of their employer-provided health insurance coverage.
The consequence was a decline in utilization of HIV diagnostic and prevention services early in the pandemic. However, the CDC notes in its report, “the full impact of the pandemic on use of HIV prevention and care services and HIV outcomes is not known.”
The CDC HIV Testing Report
CDC researchers set out to address this blind spot by analyzing changes in HIV testing, PrEP, and ART in the US from 2019 through 2021. For the laboratory testing part of the analysis, they looked at quarterly data from Labcorp, Quest Diagnostics, the IQVIA Real-World Data — Longitudinal Prescription Database, and the National HIV Surveillance System (NHSS). Analyzing combined laboratory data from Labcorp and Quest, they estimated the number of HIV tests performed during the period, using Current Procedural Terminology (CPT) codes to identify the results of HIV antigen, antibody, and RNA tests. They also used laboratory data to estimate the number of HIV viral load tests performed and what proportion of those tests indicated viral load suppression.
Published on World AIDS Day, the CDC analysis found that HIV testing fell off in the early months of the pandemic but rebounded at the end of 2020. According to the CDC, a total of 2,471,614 HIV tests were performed during the first quarter of 2020, with 8,438 persons being diagnosed with HIV infection. The second quarter of the year was the first to feel the full impact of the PHE that was declared in March. During that quarter, HIV tests performed declined 32 percent to 1,682,578, and only 6,228 persons received an HIV diagnosis, a 26 percent decrease.
But the rebound began in the third quarter of 2020 when total HIV tests increased 38 percent to 2,325,554 and 7,905 people were diagnosed with HIV (27 percent increase). HIV test totals stabilized in the last quarter of 2020 and through all four quarters of 2021.
Figure A. Total HIV Tests Performed, 2019 to 2021
| 2019 | 2020 | 2021 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 |
| 2,101,633 | 2,523,317 | 2,572,963 | 2,451,303 | 2,471,614 | 1,682,578 | 2,325,554 | 2,274,593 | 2,346,191 | 2,646,562 | 2,643,539 | 2,453,114 |
| (+20.1%) | (+2.0%) | (−4.7%) | (+0.8%) | (−31.9%) | (+38.2%) | (−2.2%) | (+3.1%) | (+12.8%) | (−0.1%) | (−7.2%) | |
Source: Recreated from CDC, “HIV Services and Outcomes During the COVID-19 Pandemic — United States, 2019–2021.” December 2022.1
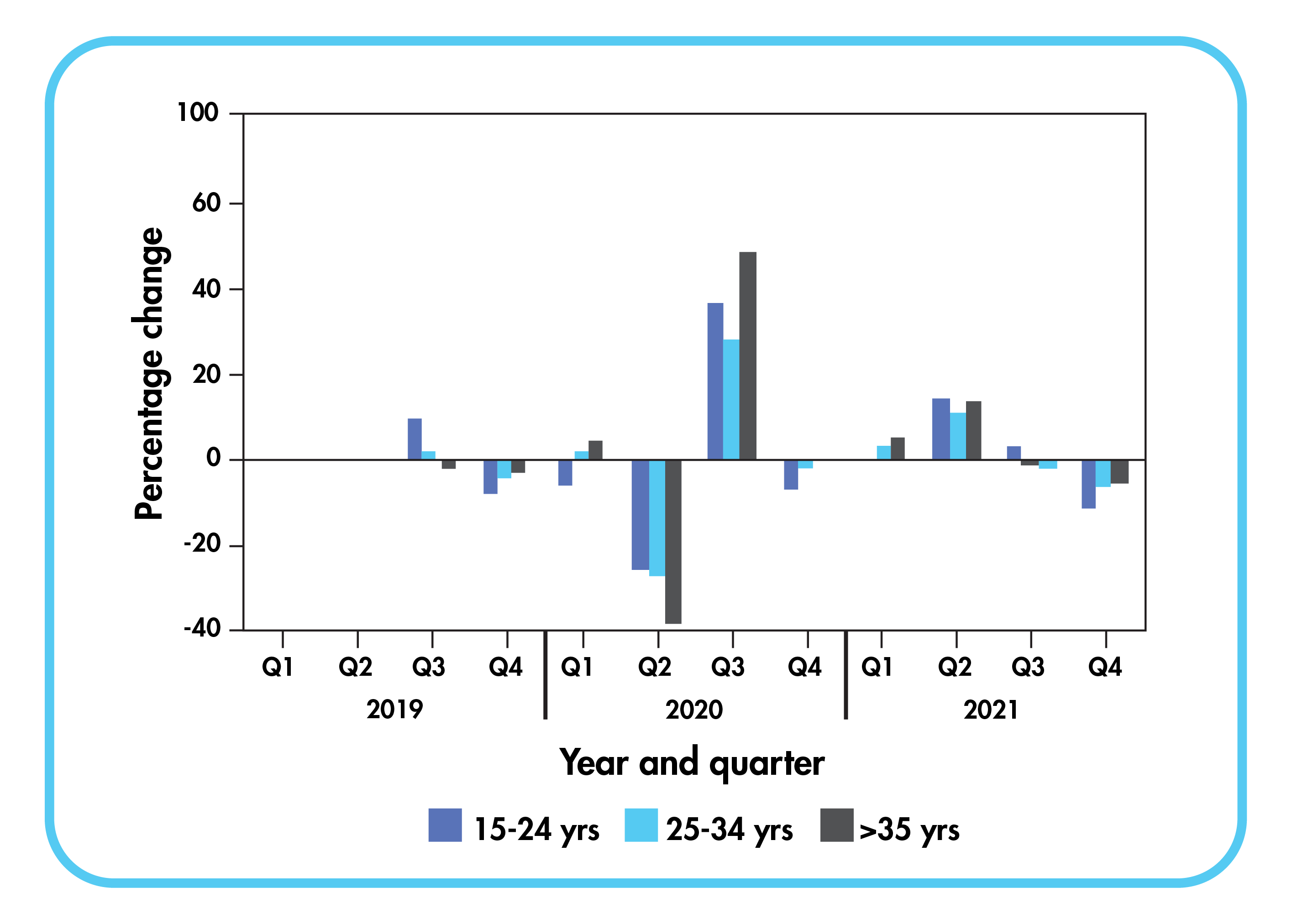
The CDC report also considered HIV testing numbers by age group. It finds that in 2020, persons ages 35 and older experienced the largest quarter-to-quarter decrease in number of HIV tests from Q1 (1,076,548) to Q2 (660,593), a decline of 39 percent.
Figure B. Total HIV Tests, 2019 to 2021, By Age Group
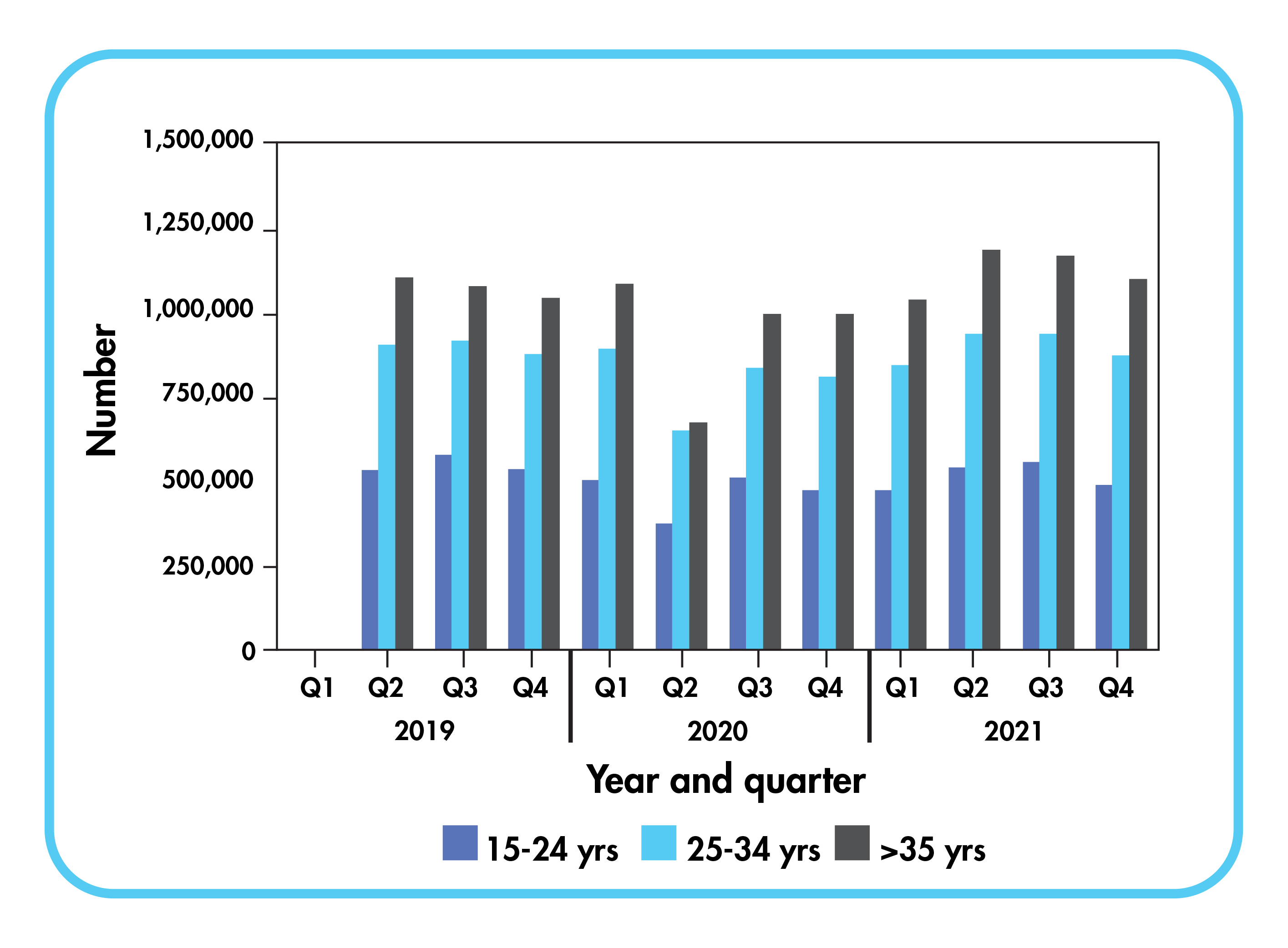
Figure C. HIV Tests Percentage Change, 2019 to 2021, By Age Group
The number of persons prescribed PrEP during the period corresponded with HIV test totals. Meanwhile, the proportion of persons linked to HIV care, the number who were prescribed ART, and the proportion with a suppressed viral load test (<200 copies of HIV RNA per mL) among those tested all remained stable during the study period.
Significance of the Findings
Overall, the HIV prevention and care system proved resilient during the pandemic, quickly bouncing back from the disruptions experienced in the early months. By the end of 2020, the system had stabilized, with HIV tests exceeding pre-pandemic levels.
“Compared with the performance of the US HIV prevention and care service system before the COVID-19 pandemic, the system performed as well as it did during the first two years of the pandemic when access to services decreased as a result of shutdowns and loss of employer-sponsored health insurance,” the CDC report concluded. So, while HIV testing and PrEP measures did fall off sharply during the second quarter of 2020, they rebounded the very next quarter. From that point on, PrEP prescriptions “followed pre-pandemic trends, increasing each quarter through 2021,” the report added.
HIV diagnoses also declined during the pandemic. While that might be attributable to decreases in HIV testing, it might also have been caused by reduced transmissions during the pandemic as a result of shutdown orders and social distancing. “Despite the decline in HIV diagnoses, similar proportions of persons receiving a diagnosis were linked to care compared with pre-pandemic proportions,” according to the CDC.
Takeaway
The CDC report suggests that the HIV prevention and care service system was resilient during the COVID-19 pandemic. However, disruptions did take place, and their long-term impact on HIV outcomes remains to be determined. The CDC recommends measures that can be taken to “ensure robust prevention services” in the event of future public health emergencies, including the development of self-test kits and nonclinical delivery models to maintain necessary levels of HIV testing and PrEP. In addition, communities and public health organizations should use “data on the impact of disrupted services and outcomes during the pandemic, along with risk behavior change data…in models to predict the impact on HIV transmission and delays in achieving goals of the EHE initiative,” the CDC said.
References:
Subscribe to Clinical Diagnostics Insider to view
Start a Free Trial for immediate access to this article