Medicare Reimbursement: CMS Proposes to Cut Part B Payments to Physicians
The proposed PFS rule also includes other changes that will affect physician, lab, and other reimbursements in 2024 and beyond.
Confirming some of the medical industry’s worst fears, the Centers for Medicare & Medicaid Services (CMS) is seeking to cut Medicare Part B physician payments in 2024. Issued on July 13, the proposed Medicare Physician Fee Schedule (PFS) rule, includes other changes that will affect physician, lab, and other reimbursements in 2024 and beyond.1
The Proposed PFS Pay Cuts
CMS has proposed a calendar year (CY) conversion factor of $32.75, which is $1.14 (3.36 percent) lower than the CY 2023 conversion factor of $33.89.2 The conversion factor reduction is based on several factors, including:3
- the expiration of the 2.5 percent payment increase mandated for CY 2023 under the Consolidated Appropriations Act of 2023 (CAA),
- the CAA-mandated one-time 1.25 percent payment increase for CY 2024,
- a 0.00 percent conversion factor update under the Medicare Access and CHIP Reauthorization Act, and
- a -2.17 percent budget-neutrality adjustment
The Practical Impact on Physicians and Labs
Cuts in the conversion factor have significant ripple effects because PFS payments are based on the relative resources used to furnish the service, expressed in relative value units (RVUs). CMS then applies the conversion factor to the RVU total to calculate an actual payment rate for the service. Thus, a lower conversion factor results in lower payment rates.
Although the size of the actual payment cut will depend on the service involved, a cut of any degree will have an adverse effect on physicians, particularly during these inflationary times. So it’s hardly surprising that physician groups and their allies have expressed discontent with the CMS proposal and called on Congress to oppose it. If adopted, the conversion rate cut “would exacerbate the financial pressures” facing physicians, given that Medicare PFS payments are already behind the pace of inflation, according to an American Medical Group Association (AMGA) statement.4
The statement emphasizes that AMGA members can’t afford this cut, expressing concern that it will force members “to make tough decisions on staffing and the services they can offer to their communities.”
A statement from American Medical Association (AMA) president Jesse Ehrenfeld, MD, MPH echoes these sentiments. “When adjusted for inflation, Medicare physician payment already has effectively declined 26 percent from 2001 to 2023 before additional inflation and these cuts are factored in,” Ehrenfeld states.5
Physician Pay and Practice Costs versus Inflation, 2001 to 2023
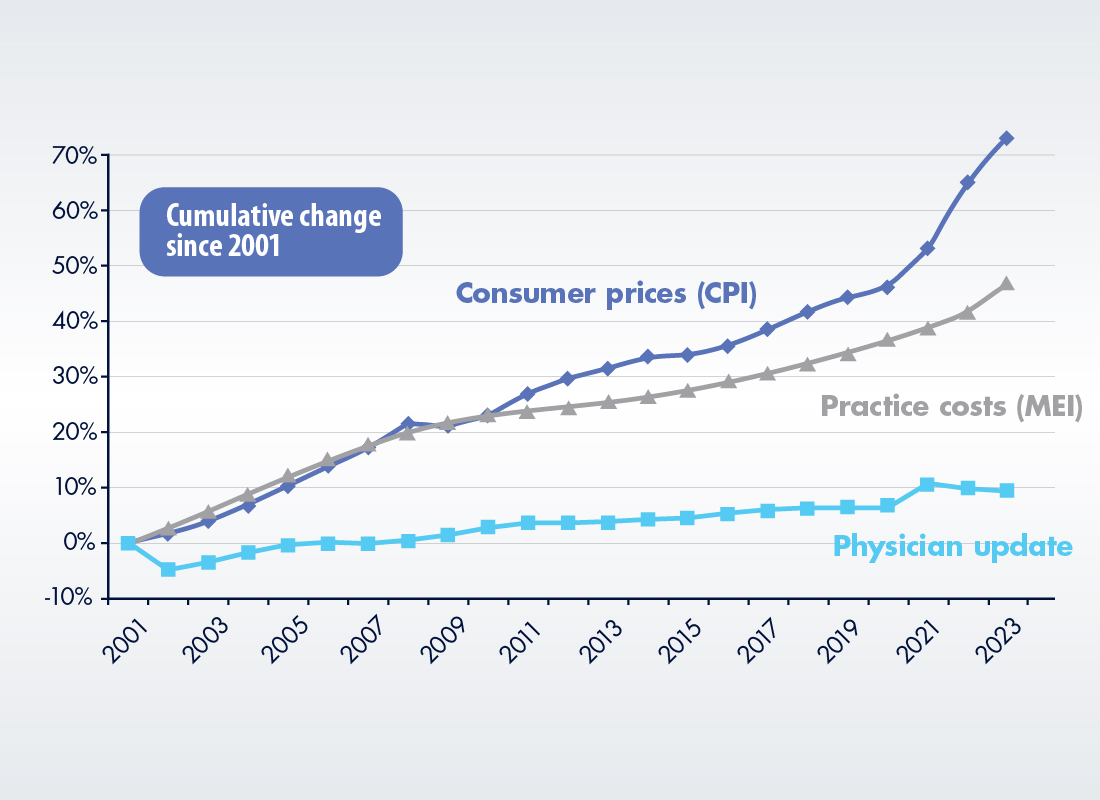
“This is almost biblical in its impact,” the AMA president adds. “Seven lean years that include a pandemic and rampaging inflation. Physicians need relief from this unsustainable journey.”5
Three Other Key Reimbursement Changes
Though the conversion rate cut is the headliner, the proposed 2024 PFS includes three other changes that could have an impact on your lab’s future Medicare Part B reimbursements:
1. Revisions to PAMA Price Reporting and Price Cuts
As required by the CAA, CMS is proposing to delay the next PAMA-mandated Clinical Laboratory Fee Schedule (CLFS) private payer rate reporting period from Q1 2023 to Q1 2024. When and if PAMA reporting resumes, it will pick up where it left off before the recent series of legislative delays—namely, with price data from January 1, 2019 to June 30, 2019.
In addition, the phase-in of the next round of PAMA CLFS price reductions would cap the maximum payment cut for a particular test at 15 percent year-on-year.
2. Delay in Split/Shared E/M Visit Billing Rule Changes
The PFS also deals with the issue of billing split or shared evaluation and management (E/M) visits in which patients in a hospital or other institutional setting receive services provided by both physicians and nonphysician practitioners (NPPs). Under Medicare rules, the visit must be billed by the physician or NPP who performs the “substantive portion” of the visit. CMS had proposed to change the definition of “substantive portion” based on visit time. Under the changed policy, if an NPP performed at least 50 percent of the E/M visit, CMS would pay only 85 percent of the PFS rate. Having delayed implementation of the new policy in 2023, CMS is now putting it off for at least one more year.
Impact: During CY 2024, providers who bill for split E/M visits will continue to have the choice of defining “substantive portion” based either on who performed one of three key components of the visit—history, exam, or medical decision-making—or on who occupied more than half of the total visit time.
3. G2211 Add-On Code for Complex Visits or Care
CMS wants to implement a separate add-on payment for Healthcare Common Procedure Coding System (HCPCS) code G2211 designed to capture the resource costs associated with E/M visits for primary care and longitudinal care of complex patients.
Impact: Effective January 1, 2024, the add-on code will be available for most outpatient office visits, but not for those that are reported with modifier 25 or bundled with another service. CMS also says that the code should not be used when the E/M visit care “is provided by a professional whose relationship with the patient is of a discrete, routine, or time-limited nature,” such as treatment for fractures or seasonal allergies.1
References:
- https://www.federalregister.gov/documents/2023/08/07/2023-14624/medicare-and-medicaid-programs-cy-2024-payment-policies-under-the-physician-fee-schedule-and-other
- https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2024-medicare-physician-fee-schedule-proposed-rule
- https://public-inspection.federalregister.gov/2023-14624.pdf
- https://www.amga.org/about-amga/amga-newsroom/press-releases/7132023_1
- https://www.ama-assn.org/press-center/press-releases/ama-medicare-physician-payment-proposal-wake-call-congress
- https://www.ama-assn.org/system/files/medicare-updates-inflation-chart.pdf
Subscribe to view Essential
Start a Free Trial for immediate access to this article