Prostate Cancer: National Guidelines Have Not Stopped Overuse of Low-Value PSA Screening in Older Males
New research suggests that the call to rein in low-value prostate cancer screening seems to be falling on deaf ears.

Prostate-specific antigen (PSA) cancer screening has the potential to save lives. However, for recipients ages 70 and older, its collective costs and risks generally outweigh its medical benefits, according to national guidelines discouraging PSA screening for this age group.1 However, new research suggests that the call to rein in low-value prostate cancer screening seems to be falling on deaf ears.
The Diagnostic Challenge
Prostate cancer is the second most frequently diagnosed cancer and fifth leading cause of cancer death in men worldwide with more than 1.276 million new cases per year. Screening can reduce prostate cancer deaths and is highly recommended for men ages 45 and older with a family history of cancer—especially for African American men.2
The effectiveness of current prostate-specific antigen (PSA) blood testing is marred by the PSA protein’s lack of reliability as a biomarker. Although high PSA levels are associated with prostate cancer, the cancer is often low-grade and poses no threat to the patient. High PSA levels may also indicate infection, inflammation, or other less threatening diseases.3 But because of the risks involved, physicians commonly order biopsies for patients whose screening tests show high PSA levels to rule out the risk of cancer.4 As a result of this better-safe-than-sorry strategy, many men experience anxiety and undergo costly and invasive procedures that can result in erectile dysfunction or urinary incontinence while yielding no medical benefits.1
For these reasons, one of the most influential sources of guidance for diagnostic testing, the U.S. Preventive Services Task Force (USPSTF), revised its guidelines in 2018 to recommend that males ages 55 to 69 make their own personal decision about whether to undergo PSA screening after talking to their physician about the risks and benefits involved. The USPSTF also advises against PSA screening for prostate cancer in men ages 70 and older due to the risks of false positives and overdiagnosis of indolent disease. The latter is a D recommendation, meaning that physicians are advised to discourage men 70 and older from seeking PSA screening.1
Older Men Are Still Being Overscreened for Prostate Cancer
Despite the revised USPSTF recommendations, there is evidence that prostate cancer overscreening in older men is still taking place. To test this hypothesis, a group of researchers from the University of California San Diego (UCSD) analyzed data from the 2020 Behavioral Risk Factor Surveillance System (BRFSS), a nationwide phone survey of US adults conducted by the Centers for Disease Control and Prevention (CDC) that looks at utilization of preventive services for chronic illnesses based on behavioral risk factors.5
After excluding those with a former or current prostate cancer diagnosis, the researchers assembled a cohort consisting of 32,306 male respondents, of which 87.6 percent were White, 4.3 percent Black, 3.4 percent Hispanic, 1.2 percent Asian, and 1.1 percent American Indian. The cohort was classified into three age groups:
-
- 70 to 74 years (42.8 percent)
-
- 75 to 79 years (28.4 percent)
- 80 years and older (28.9 percent)
The researchers used weighted multivariable logistic regressions and two-sided significance tests to characterize factors associated with recent screening, defined as PSA testing within the past two years.
The UCSD Study Findings
Published in the April 11, 2023 issue of JAMA Network Open, the UCSD study finds that older males in the US are still being overscreened for prostate cancer. Specifically, recent PSA screening rates were:
-
- 55.3 percent for the 70-to-74-year age group;
-
- 52.1 percent for the 75-to-79-year age group; and
- 39.4 percent for the 80-year-or-older age group.
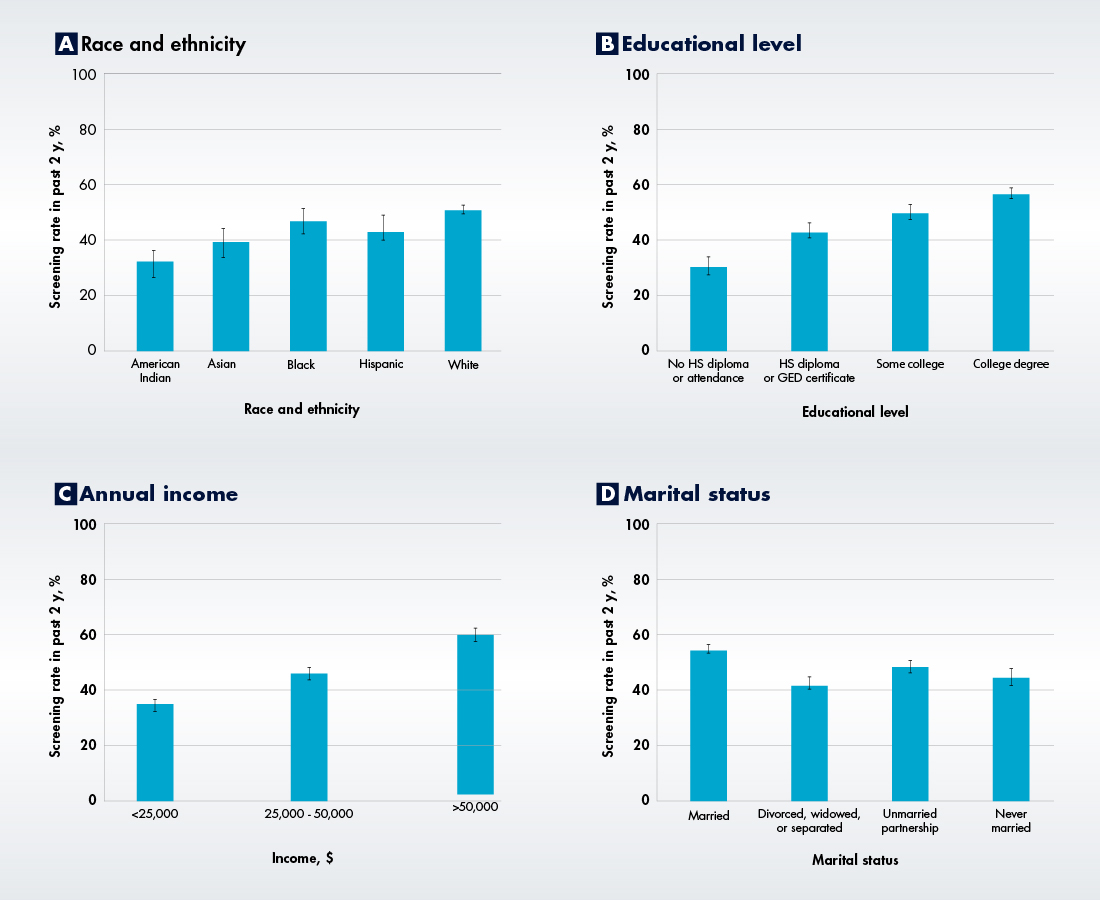
The researchers also found that White males had the highest screening rate (50.7 percent) while American Indian males had the lowest (32.0 percent). Married men were screened more than unmarried men, as were men that had a primary care physician (PCP), a post-high school educational level, and an income level above $25,000 per year.
Screening Rates by Race/Ethnicity, Education Level, Annual Income, and Marital Status
Takeaway and Significance
The new UCSD study suggests that the 2018 USPSTF guidelines advising against PSA prostate cancer screening in males over age 70 have not taken hold. The study also offers clues as to why overscreening is taking place and how it may be prevented. The researchers found that discussing PSA testing benefits with a clinician was associated with increased screening. The good news from that finding is that it indicates that physicians have an influence on patient testing decisions; the bad news is the suggestion that physicians might be encouraging PSA screening in older men, rather than discouraging it as the USPSTF guidelines advise.
More action may be necessary to disincentivize low-value PSA prostate cancer screening at the recommended age 70 cutoff, the UCSC researchers conclude. The fact that physicians seem to have influence over the testing decisions made by older men suggests that “changes could be made at the clinician level to increase adherence to age-based PSA testing guidelines.”
Another potentially significant finding from the study relates to the types of older male patients who are most likely to seek low-value PSA screening, namely, those who have regular contact with a PCP, higher educational levels, and higher annual incomes. The good news is that these very same factors could make overutilizers more receptive to direct patient education that explains the risks and diminished benefits offered by low-value screening. The researchers call for further work to quantify the implications of overscreening and especially the consequences of overtreatment for patients.
Among the limitations the study authors note is that the BRFSS survey data divides respondents by five-year age intervals without specifying their exact ages, meaning some respondents may have fallen within the age range recommended for screening. The survey also fails to distinguish between PSA testing for prostate cancer screening as opposed to PSA testing for monitoring purposes.
In addition, the authors acknowledge that the BRFSS survey had a response rate of only 47.9 percent and some states did not offer the survey’s prostate cancer module, thus creating the potential for selection bias and limiting the generalizability of the data. However, the authors used several methodological methods to address these data limitations.
References:
Subscribe to Clinical Diagnostics Insider to view
Start a Free Trial for immediate access to this article